© 2006 All Rights Reserved. Do not distribute or repurpose this work without written permission from the copyright holder(s).
Printed from https://danginteresting.com/cancer-assassins/
In the USA and other developed countries, cancer is presently responsible for about 25% of all deaths. The human immune system employs a network of microscopic sentries to watch for all manner of diseases, including the malformed, rapidly-dividing cells which make up cancer. But sometimes the immune system’s somewhat lackadaisical response to cancer cells allows the rogue cells to overwhelm the immune system, posing a deadly threat to the body.
Conventional cancer treatments such as chemotherapy and radiation therapy can injure and kill these tumor cells, but with an inevitable degree of collateral damage. By way of example, chemotherapy has a therapeutic index of six to one, meaning that one healthy cell is killed for every six cancer cells which are destroyed. Given that tumors can be made up of millions of cells, the incidental damage caused by chemotherapy is considerable. Radiation therapy has the same drawback.
Clearly these radiation and specialized-poison therapies are highly indiscriminate treatments, but they are the best that modern medicine’s cancer-fighting toolbox has to offer. But science is working hard to develop an army of microscopic agents which can hunt down and destroy cancer cells with decisive prejudice: antitumor viruses.
Pitting viruses against cancer cells is not a new idea. In the early 1900s doctors began to take note of the fact that patients’ tumors tended to regress when a patient contracted a viral disease. But there was no means to harness this knowledge, since introducing harmful viruses into an already compromised individual was a dangerous prospect. Much later, in 1956, researchers deliberately introduced adenovirus— the virus responsible for the common cold— into thirty patients with cervical cancer. Many of the tumors shrunk as a result, but once the immune system began eliminating the virus from the patients’ systems the tumors began to grow again.
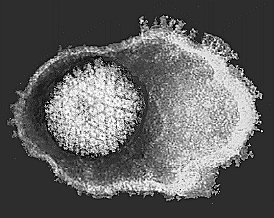
Normally, when a virus encounters a cell which it can infect, it injects its genetic material into the cell. The cell’s enzymes react to the new genetic material by setting to work replicating it, essentially building copies of the original virus. In most cases, the thousands of resulting viruses then breach the cell membrane to escape, which kills the cell. Each of these viruses can then move on to repeat the process in other cells. Once the invaders are discovered and identified, the immune system usually reacts by raising the body temperature to slow down cell processes (fever), then sending in white blood cells to eliminate the viruses.
Advances in virus-handling techniques are allowing scientists to refashion viruses from agents of destruction into useful instruments. Gene therapy uses specially prepared viruses to deliver genetic payloads into cells; these viruses are preloaded with the desired genes, and they are modified in such a way that they are prevented from multiplying. The viruses then insert the genes into target cells and die off without killing the host cell. But multiple treatments are problematic, since the immune system recognizes the viruses from the previous treatment, and quickly eliminates them. Researchers are now experimenting with immunosuppressant drugs to delay the immune system’s reaction, as well as some physical modifications to the viruses which help them to evade the immune response.

In 1999, scientists used a modified adenovirus to deliver a gene called “p53” to the lung tumors of twenty-five individuals. A malignant cancer cell is often prevented from entering the natural cell-death phase due to a malformed p53 gene, allowing them to outproduce and outlive normal cells. Using viruses to replace the mutated gene with a normal gene reduced or stopped the tumor growth in eighteen of the twenty-five patients. A similar method has been tested in lab animals where viruses indiscriminately deliver a gene which does no harm to normal cells, but causes cancer cells to die. Where chemotherapy offers a therapeutic index of six to one, these methods have demonstrated indexes of about 10,000 to one in the laboratory.
A more recent approach takes advantage of a virus’s main strength: its propensity for replication. Laboratory-built, submicroscopic assassins have been derived from viruses which are modified so they can only infect cancer cells. These viruses can simply be let loose upon the patient, killing only tumor cells until there are none left to infect. Additionally, the viruses can be equipped with genetic payloads which boost the body’s immune response to the cancer; this effect may actually act as a vaccine against future cancer cells of the same type, since the body’s immune reaction to those cells will be increased.
Because every virus can only infect certain cell types, a whole array of customized cancer-killers would be necessary to address a wide variety of cancers. The adenovirus which causes the common cold can be used against many types of tumors, and has shown impressive results. In August of 2000, a team headed by Fadlo R. Khuri of the Texas Medical Center in Houston reported that twenty-five of thirty patients with advanced head and neck cancer responded favorably to a combination of chemotherapy and a modified adenovirus… in fact the tumors in eight patients disappeared entirely. Adenovirus would be useless against brain tumors due to the blood-brain barrier, however a modified herpesvirus— a disease which infects the nervous system— has been tested against brain tumors in human trials with encouraging early results.
Although the modified viruses would have their harmful payloads removed, thus preventing them from causing the diseases which they typically trigger, there are naturally some risks involved in utilizing viruses… particularly those which are tailored to sidestep our immune systems. Such a virus might mutate into something harmful, posing a greater risk than that from which it originated. But with proper research and testing, perhaps those risks can be mitigated to levels similar to that of vaccinations. In time, after years of experiments, testing, and trials, a typical cancer treatment may involve an injection of modified viruses in concert with chemotherapy and/or radiation therapy, with a cure rate near 100%.
© 2006 All Rights Reserved. Do not distribute or repurpose this work without written permission from the copyright holder(s).
Printed from https://danginteresting.com/cancer-assassins/
Since you enjoyed our work enough to print it out, and read it clear to the end, would you consider donating a few dollars at https://danginteresting.com/donate ?